Congestive Heart Failure (CHF) is a critical, life-altering condition that affects millions worldwide. As a complex clinical syndrome, CHF results from any structural or functional cardiac disorder that impairs the ventricle’s ability to fill with or eject blood effectively. In this comprehensive article, we delve deep into the causes, symptoms, stages, diagnosis, and treatment of congestive heart failure to provide a robust resource for patients, caregivers, and healthcare professionals alike.
What Is Congestive Heart Failure?
Congestive Heart Failure occurs when the heart is unable to pump blood efficiently to meet the body’s demands. This leads to a buildup of fluid (congestion) in the lungs, liver, gastrointestinal tract, and extremities.
There are two major types:
Left-sided heart failure: Most common type; leads to fluid backing up into the lungs (pulmonary congestion).
Right-sided heart failure: Often caused by left-sided failure; fluid may back up into the abdomen, legs, and feet.
Heart failure can also be categorized based on ejection fraction (EF):
Heart Failure with Reduced Ejection Fraction (HFrEF): EF ≤ 40%
Heart Failure with Preserved Ejection Fraction (HFpEF): EF ≥ 50%
Common Causes and Risk Factors of CHF
CHF is often the end result of other cardiovascular diseases. The most common causes include:
Coronary artery disease (CAD): Blocked arteries reduce blood flow to the heart.
Hypertension (High blood pressure): Forces the heart to work harder.
Myocardial infarction (heart attack): Damages heart muscle.
Cardiomyopathy: Disease of the heart muscle.
Valvular heart disease: Dysfunctional heart valves disrupt blood flow.
Other contributing risk factors:
Diabetes
Obesity
Chronic kidney disease
Sleep apnea
Smoking
Excessive alcohol or drug use
Family history of heart disease
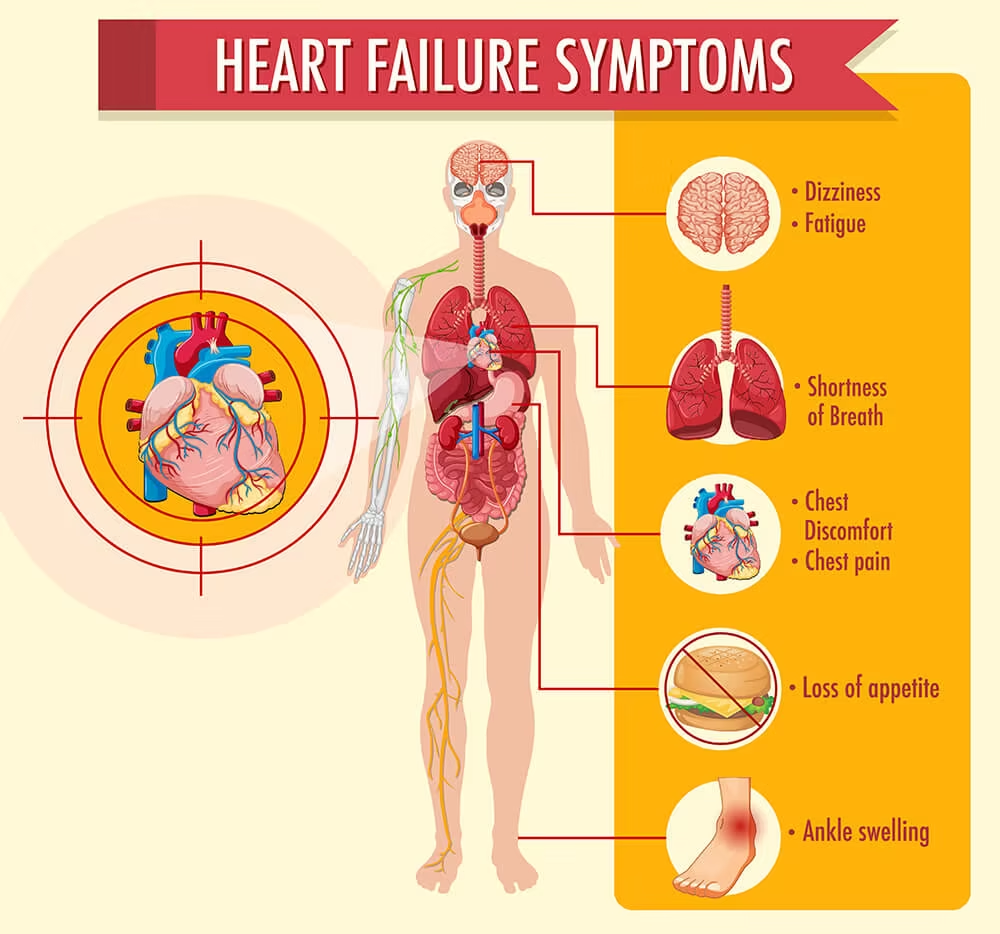
Recognizing the Symptoms of Congestive Heart Failure
CHF symptoms vary depending on the type and severity of the condition. Early recognition is crucial for timely intervention.
Common Symptoms:
Shortness of breath (dyspnea), especially during exertion or lying flat
Persistent cough or wheezing, often with white or pink blood-tinged phlegm
Fatigue and weakness
Swelling (edema) in legs, ankles, and feet
Rapid or irregular heartbeat
Sudden weight gain from fluid retention
Ascites (abdominal swelling)
Increased need to urinate at night
Reduced ability to exercise
Stages of Congestive Heart Failure
The American Heart Association and American College of Cardiology classify heart failure into four stages (A to D):
Stage A: At high risk for CHF but without structural heart disease or symptoms.
Stage B: Structural heart disease present but without signs or symptoms.
Stage C: Structural heart disease with prior or current symptoms.
Stage D: Refractory CHF requiring specialized interventions.
The New York Heart Association (NYHA) classification further categorizes patients based on symptom severity (Class I–IV).
How Is CHF Diagnosed?
Proper diagnosis is critical for managing CHF effectively. A comprehensive assessment includes:
Medical History & Physical Exam:
Evaluation of symptoms, risk factors, family history
Listening for heart murmurs, lung congestion, swelling
Diagnostic Tests:
Echocardiogram: Key test to evaluate heart structure and function
Electrocardiogram (ECG): Detects arrhythmias or ischemia
Chest X-ray: Shows heart size and lung fluid
BNP or NT-proBNP blood test: Measures levels of brain natriuretic peptide, elevated in CHF
Cardiac MRI or CT scan: Detailed heart imaging
Stress testing: Evaluates heart performance under exertion
Cardiac catheterization: Identifies coronary blockages
Treatment Options for Congestive Heart Failure
CHF requires a multifaceted treatment approach tailored to individual needs. Treatment goals include improving symptoms, slowing disease progression, and reducing hospitalizations.
Lifestyle Modifications:
Low-sodium diet
Fluid restriction
Regular physical activity as tolerated
Weight monitoring
Smoking cessation
Limiting alcohol intake
Medications:
ACE inhibitors/ARBs: Lower blood pressure and reduce heart workload
Beta-blockers: Slow heart rate and improve function
Diuretics: Reduce fluid buildup
Aldosterone antagonists: Help eliminate excess sodium and water
SGLT2 inhibitors: Proven to benefit HFrEF patients
Digoxin: Helps improve heart pumping in select cases
Advanced Therapies:
Implantable cardioverter-defibrillators (ICDs): Prevent sudden cardiac death
Cardiac resynchronization therapy (CRT): Coordinates heart contractions
Left ventricular assist devices (LVADs): Mechanical support for advanced CHF
Heart transplantation: Last resort for end-stage CHF
Preventing Congestive Heart Failure
Prevention starts with managing risk factors and adopting heart-healthy habits:
Control blood pressure and cholesterol
Manage diabetes effectively
Maintain a healthy weight
Exercise regularly
Avoid smoking and excessive alcohol
Follow a heart-healthy diet (DASH or Mediterranean diet)
Early detection and treatment of conditions like CAD and hypertension can significantly reduce the risk of developing CHF.
Living with CHF: Prognosis and Quality of Life
While CHF is a chronic condition, many patients lead fulfilling lives with proper management. Regular follow-ups with a cardiologist, medication adherence, and self-care can drastically improve outcomes. Monitoring symptoms daily and knowing when to seek medical help are essential to avoid complications.
The prognosis depends on the stage at diagnosis, underlying causes, response to treatment, and patient compliance. With advances in medicine and technology, many patients live longer and better than ever before.
Conclusion
Congestive Heart Failure is a complex but manageable condition when approached with a comprehensive strategy. From recognizing early symptoms to applying advanced treatments, the key lies in timely intervention and consistent care. Whether you’re a patient, caregiver, or healthcare provider, staying informed and proactive can make a significant difference in outcomes.